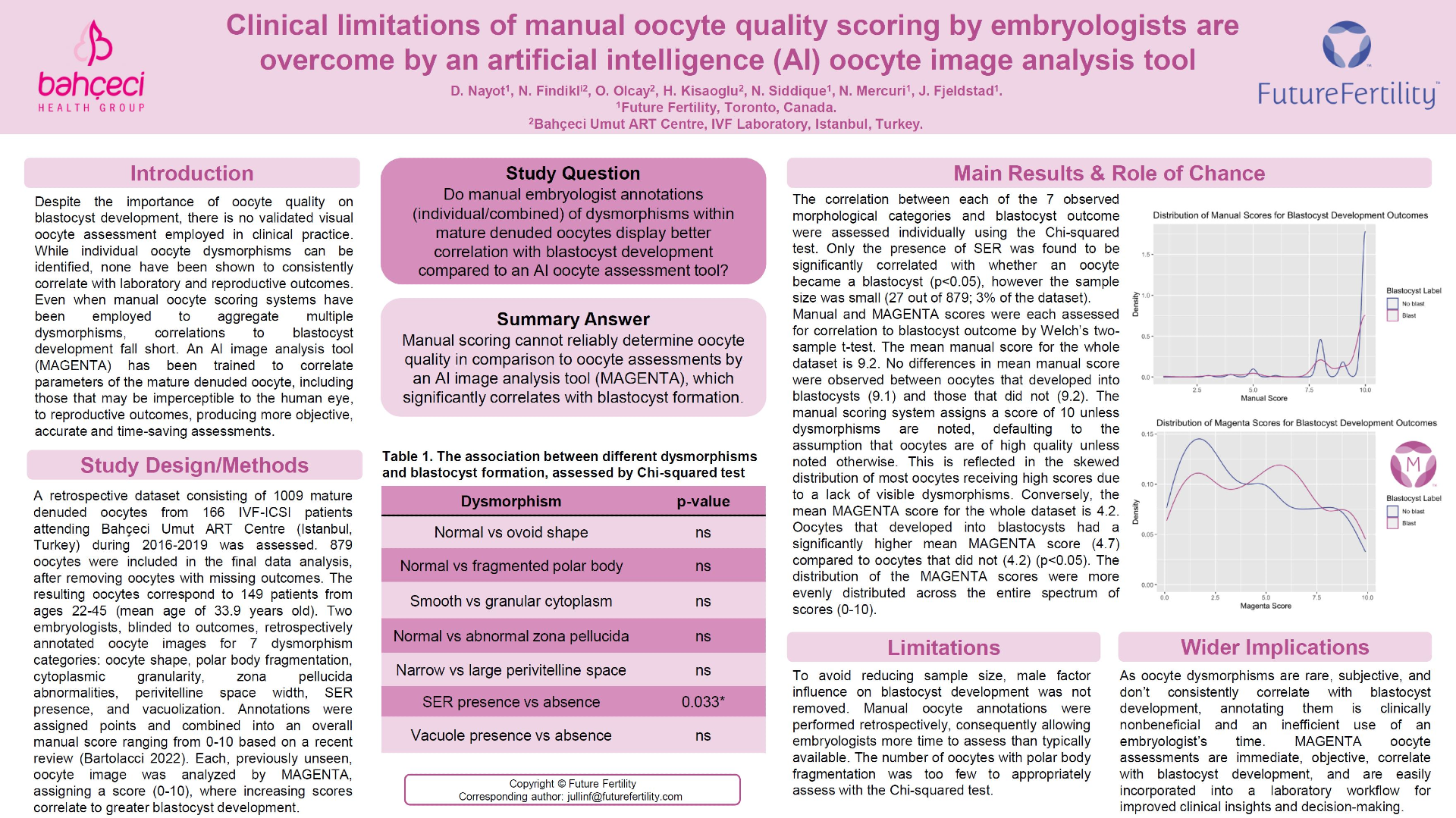
STUDY QUESTION:
Do manual embryologist annotations (individual/combined) of dysmorphisms within mature denuded oocytes display better correlation with blastocyst development compared to an AI oocyte assessment tool?
SUMMARY ANSWER:
Manual scoring cannot reliably determine oocyte quality in comparison to oocyte assessments by an AI image analysis tool (MAGENTA), which significantly correlates with blastocyst formation.
WHAT IS KNOWN ALREADY:
Despite the importance of oocyte quality on blastocyst development, there is no validated visual oocyte assessment employed in clinical practice. While individual oocyte dysmorphisms can be identified, none have been shown to consistently correlate with laboratory and reproductive outcomes. Even when manual oocyte scoring systems have been employed to aggregate multiple dysmorphisms, correlations to blastocyst development fall short. An AI image analysis tool (MAGENTA) has been trained to correlate parameters of the mature denuded oocyte, including those that may be imperceptible to the human eye, to reproductive outcomes, producing more objective, accurate and time-saving assessments.
STUDY DESIGN:
A retrospective dataset consisting of 1009 mature denuded oocytes from 166 IVF-ICSI patients attending Bahçeci Umut ART Centre (Istanbul, Turkey) during 2016-2019 was assessed. 879 oocytes were included in the final data analysis, after removing oocytes with missing manual morphological assessments, lab outcomes (fertilization and blastocyst development), or whose static images could not be linked to outcomes. The resulting 879 oocytes correspond to 149 patients from ages 22-45 (mean age of 33.9 years old).
METHODS:
Two embryologists, blinded to outcomes, retrospectively annotated oocyte images for 7 dysmorphism categories: shape/size, cytoplasmic granularity, polar body fragmentation, zona pellucida thickness, perivitelline space thickness, smooth endoplasmic reticulum (SER) presence, and vacuole presence. Annotations were assigned points and combined into an overall manual score ranging from 0-10 based on a recent review (Bartolacci 2022). Each, previously unseen, oocyte image was analyzed by MAGENTA, assigning a score (0-10), where increasing scores correlate to greater blastocyst development.
MAIN RESULTS AND THE ROLE OF CHANCE:
The correlation between each of the 7 observed morphological categories and blastocyst outcome were assessed individually using the Chi-squared test. Only the presence of SER was found to be significantly correlated with whether an oocyte became a blastocyst (p<0.05), however the sample size was small (27 out of 879; 3% of the dataset).
Manual and MAGENTA scores were each assessed for correlation to blastocyst outcome by Welch’s two-sample t-test. The mean manual score for the whole dataset is 9.2. No differences in mean manual score were observed between oocytes that developed into blastocysts (9.1) and those that did not (9.2). The manual scoring system assigns a score of 10 unless dysmorphisms are noted, defaulting to the assumption that oocytes are of high quality unless noted otherwise. This is reflected in the skewed distribution of most oocytes receiving high scores due to a lack of visible dysmorphisms. Conversely, the mean MAGENTA score for the whole dataset is 4.2. Oocytes that developed into blastocysts had a significantly higher mean MAGENTA score (4.7) compared to oocytes that did not (4.2) (p<0.05). The distribution of the MAGENTA scores were more evenly distributed across the entire spectrum of scores (0-10).
LIMITATIONS & REASONS FOR CAUTION:
To avoid reducing sample size, male factor influence on blastocyst development was not removed. Manual oocyte annotations were performed retrospectively, consequently allowing embryologists more time to assess than typically available. The number of oocytes with polar body fragmentation was too few to appropriately assess with the Chi-squared test.
WIDER IMPLICATIONS OF THE FINDINGS:
Because oocyte dysmorphisms are rare, subjective, and don’t consistently correlate with blastocyst development, annotating them is clinically nonbeneficial and an inefficient use of an embryologist’s time. MAGENTA oocyte assessments are immediate, objective, correlate with blastocyst development, and are easily incorporated into a laboratory workflow for improved clinical insights and decision-making.
You Might Also Like …
Join our mailing list for dispatches on the future of fertility