In IVF, poor blastocyst development is often attributed to poor egg quality. However, MAGENTA™ enables a more objective, image-based assessment by providing measureable insights into oocyte quality. When MAGENTA™ scores are favorable but blastulation remains suboptimal, it may prompt a deeper investigation into sperm quality, even when standard semen analysis results appears normal.
SAMPLE PATIENT CASE:
PATIENT BACKGROUND:
- 36-year-old female, G1P0 (1 termination after a spontaneous pregnancy 4 years ago with a different partner)
- Secondary infertility; trying to conceive > 2 years
- Regular ovulatory cycles; BMI 24
- AMH 3.8 ng/mL; AFC 18
PARTNER BACKGROUND:
- 39-year-old male
- Normal semen analysis per WHO 6th Edition (volume, count, motility, morphology)
- No known medical history
Following unsuccessful low-level interventions (ovarian stimulation and IUI), the couple transitioned to IVF.
IVF CYCLE OVERVIEW:
- Antagonist protocol with 225 IU FSH + 75 IU LH daily
- Triggered with GnRH agonist; freeze-all cycle planned
- 16 oocytes retrieved; 13 mature (MII)
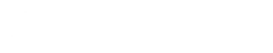
- MAGENTA™ results: 11/13 mature oocytes (85%) scored in medium-high or high quality categories
- 12 oocytes fertilized successfully via ICSI
- Unexpectedly, only 2 blastocysts developed and were cryopreserved; all other embryos arrested before Day 5.
MAGENTA™ INSIGHTS: EGG QUALITY VS. OUTCOME:
Despite excellent MAGENTA™ scores suggesting high-quality oocytes, the blastocyst rate was unexpectedly poor. This discrepancy prompted further investigation into sperm quality, even in the presence of a normal semen analysis.
Functional sperm parameters that may contribute to poor embryo development include DNA fragmentation, oxidative stress, and sperm epigenetic abnormalities, none of which are evaluated in standard semen analysis. It is estimated that up to 10% of men with infertility have elevated DNA fragmentation levels despite normal semen parameters. [Ref.1]
Both ASRM and ESHRE acknowledge [Ref.2-3] that elevated sperm DNA fragmentation (SDF) can adversely affect outcomes in IVF and ICSI, including lower fertilization and blastulation rates and higher miscarriage risk. [See references below.]
THE MAGENTA™ REPORT:
CLINICAL VALUE OF MAGENTA™ IN THIS CASE:
- Supports deeper male factor investigation: Encouraged the clinical team to go beyond standard semen analysis and consider more advanced sperm testing.
- Shifts focus from egg to sperm: Prevented incorrect attribution to the suboptimal outcome to egg quality and allowed for better-targeted counselling and next-step planning.
- Informs future treatment: The couple elected to move forward with sperm quality optimization (lifestyle; antioxidant supplements) and preparation techniques (e.g., microfluidic sperm sorting) with their second IVF cycle.
PATIENT COUNSELLING TIPS:
- Use MAGENTA™ to explain that high-quality oocytes were not the limiting factor to their suboptimal IVF outcome.
- Emphasize that sperm factors, particularly at the molecular level, can significantly influence blastulation, even when standard semen parameters are normal.
- Reassure patients that identifying the root issue allows for more personalized and effective strategies in future cycles.
If you would like to provide feedback on your counselling experience using this guidance, or other aspects related to your use of Future Fertility’s egg quality assessments, please share it with us at info@futurefertility.com.
REFERENCES
- Yang T, Yu L, Xu J, Ying L, Jia Y, Zheng Y, Zhou B, Li F. Correlation between standard sperm parameters and sperm DNA fragmentation from 11,339 samples. Syst Biol Reprod Med. 2024 Dec;70(1):91-100. doi: 10.1080/19396368.2024.2333285. Epub 2024 Apr 17. PMID: 38630599.
- Diagnosis and treatment of infertility in men: AUA/ASRM guideline part I. 2020. American Society for Reproductive Medicine.
- ESHRE Guideline Group on RPL; Bender Atik R, Christiansen OB, Elson J, Kolte AM, Lewis S, Middeldorp S, Mcheik S, Peramo B, Quenby S, Nielsen HS, van der Hoorn ML, Vermeulen N, Goddijn M. ESHRE guideline: recurrent pregnancy loss: an update in 2022. Hum Reprod Open. 2023 Mar 2;2023(1):hoad002. doi: 10.1093/hropen/hoad002. PMID: 36873081; PMCID: PMC9982362.
You Might Also Like …
Join our mailing list for dispatches on the future of fertility