THE PURPOSE OF VIOLET™
VIOLET™ reports provide you with individualized patient insights about oocyte quality to support the planning of future cryopreservation cycles. They also help you to better manage patients’ expectations for success versus general standard of care estimations. This supports your counselling conversations and the patient’s consideration of additional cryopreservation cycles to accumulate more oocytes, thus improving their cumulative success rate.
HOW VIOLET™ REPORTS WORK TO STANDARDIZE OOCYTE ASSESSMENT
Currently, there is no standardized oocyte scoring system, so reliance has been placed on age and number of MII oocytes to predict oocyte “quality”. Embryologists are unable to consistently predict blastocyst outcomes through visual assessment of oocyte morphology. Our research has determined that there is even inter- and intra-observer prediction variability.
Future Fertility technology uses AI to assess 2D images of fresh oocytes – detecting features invisible to the human eye – to predict the likelihood of blastocyst formation for each oocyte. This is coupled with statistical modelling to provide predictions of live birth. Our model was trained with more than 150,000 oocyte images and their outcomes from partnering clinics in eight countries. Future Fertility AI outperforms the accuracy of embryologists in predicting blastocyst formation by 20%, on average.1
WHAT’S IN THE REPORT?
VIOLET™ reports provide an objective measure of oocyte quality, including images and individualized predictions of blastocyst formation for each oocyte. A Personalized Live Birth prediction is also displayed for the total cohort of oocytes evaluated. These predictions are presented for comparison alongside a General Live Birth prediction (current standard of care), which is based only on age and number of mature oocytes. For patients conducting multiple cryopreservation cycles, an amalgamated VIOLET™ Summary report can be generated to deliver cumulative outcome predictions.
THE VALUE OF PERSONALIZED PREDICTIONS
General oocyte outcome calculators have historically been used by clinicians to drive decisions about the number of cycles required to achieve sufficient oocyte reserves for future success. However, focusing only on age and the number of oocytes frozen assumes that all patients of the same age have the same health status and will achieve the same outcomes, while also assuming that all oocytes from one person are of equal quality. Our research has proven that age alone is not an accurate indicator of success. As such, VIOLET™ predictions are provided alongside each oocyte image, and generally differ across oocytes in the same cycle.
VIOLET™ provides more personalized predictions because it is analyzing images of individual oocytes at the pixel-level and can therefore identify patterns that are undetectable to the human eye.
NAVIGATING THE REPORT
The front page of the VIOLET™ report provides summary predictions for your patient’s cycle(s) while the remaining pages provide individual oocyte images alongside their respective blastocyst predictions.
Blastocyst predictions: Your patient’s chances of developing blastocysts, based on our AI-powered image analysis. Calculations assume a normal semen analysis and no specific uterine receptivity issues.1-5
- • Page 1 provides overall blastocyst predictions for the full cohort of mature oocytes evaluated, based on our prediction assessment and other relevant statistics, such as the effects of cryopreservation on oocyte quality.
- • Subsequent pages provide an individual blastocyst prediction alongside each oocyte image.
Live Birth predictions:
- • Personalized prediction: The probability of achieving a live birth from the mature oocytes evaluated, based on the VIOLET™ prediction assessment and statistical modeling that accounts for egg thawing survival rates, euploid rates based on age, and clinical pregnancy rates per euploid, among other variables.
- • General prediction: A general estimate of live birth for comparison, based only on age and number of mature oocytes frozen.6 This calculation approach is the same as various online egg calculators.
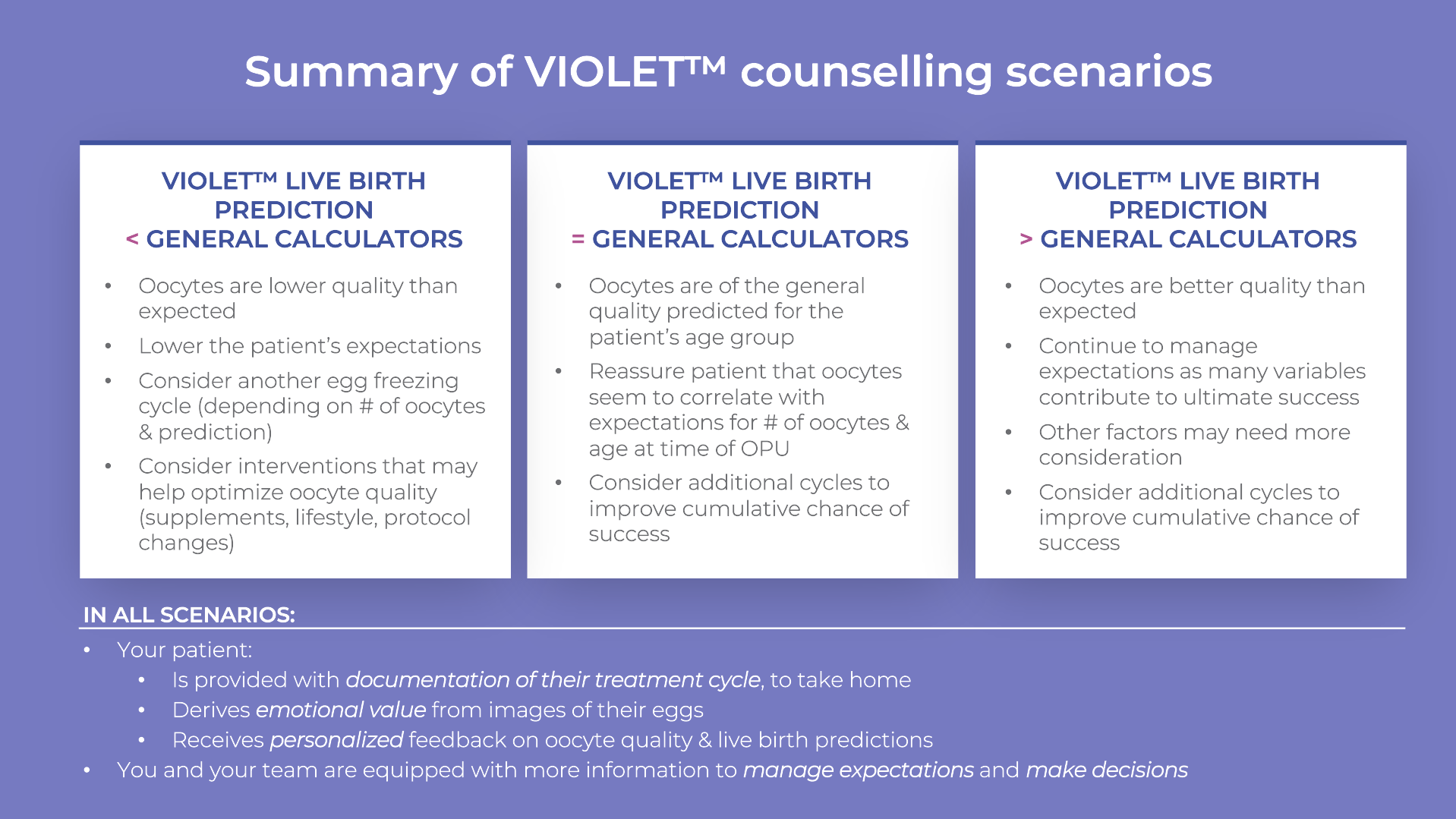
COUNSELLING SCENARIOS
When using VIOLET™ reports to counsel your patients, our recommendation is to focus on comparing the personalized insights to generalized predictions to either confirm expectations and treatment decisions or modify expectations and identify opportunities to optimize outcomes. As published patient accounts continue to arise regarding misperceptions of their chances of success (i.e., this article by the New York Times), you can help to proactively set more realistic expectations using individualized insights from VIOLET™.
1. VIOLET™ LIVE BIRTH PREDICTION IS LOWER THAN THE GENERAL PREDICTION:
Counselling actions and next steps:
- • Manage your patient’s expectations:
- – The VIOLET™ prediction is lower than you or your patient may expect (i.e., based on their age).
- – Provide transparency to your patient by highlighting these personalized insights to help manage their expectations of success.
- • Consider another cryopreservation cycle (depending on the number of oocytes and their respective predictions; also consider your patient’s financial situation).
- • Consider interventions that may help optimize oocyte quality (such as dietary supplements, lifestyle changes, treatment protocol adjustments, etc.)
Summary: In this scenario, VIOLET™ has enabled you to identify challenges with oocyte quality early on so you can recommend further cryopreservation cycles to accumulate oocytes. You can also use this assessment as a baseline for communicating changes in oocyte quality over multiple cycles and to evaluate your optimization decisions.
2. VIOLET™ LIVE BIRTH PREDICTION IS SIMILAR TO THE GENERAL PREDICTION:
Counselling actions and next steps:
- • Confirm standard of care expectations with your patient:
- – Share with your patient that their personalized oocyte assessment is consistent with expectations based on their age and number of oocytes at the time of OPU.
- • Discuss the option of additional cycles to accumulate more eggs and improve the patient’s cumulative chance of success.
- – VIOLET™ Summary reports enable you to understand cumulative blastocyst and live birth predictions over multiple cycles.
- • Provide a copy of the VIOLET™ report to the patient that they may take home as documentation of their treatment and an ongoing reminder of what to expect when they come back to use their frozen oocytes.
Summary: In this scenario, the predictions have not changed versus standard of care, but you are providing your patient with more personal, transparent information about their reproductive health. This new information enables you to discuss the option of additional cycles to accumulate more eggs and improve the patient’s cumulative chance of success. The VIOLET™ report is also a tangible take-home document providing images of your patient’s oocytes and personalized insights that they can keep on-hand for future reference.
3. VIOLET™ LIVE BIRTH PREDICTION IS HIGHER THAN THE GENERAL PREDICTION:
Counselling actions and next steps:
- • Inform your patient that their oocyte quality is better quality than expected:
- – Based on their personalized assessment, your patient’s oocyte quality is above average.
- – According to our research, age alone is not the strongest predictor of oocyte quality. While your patient has higher-than-expected oocyte quality, this still does not mean success is guaranteed (see next point).
- • Continue to manage your patient’s expectations, as multiple variables contribute to ultimate success:
- – VIOLET™ calculations assume a normal semen analysis and no specific uterine receptivity issues.
- – While VIOLET™ reports are better than embryologists at predicting blastocyst outcomes for oocytes, this AI technology is still evolving and is not 100% accurate.
- • Continue to plan future cycles to reach a cumulative live birth prediction that aligns as closely as possible with your patient’s goals and budget.
- – For example, a VIOLET™ prediction of 40% Live Birth versus a 30% general prediction is certainly an improvement in expected oocyte quality, however it also means that VIOLET™ still predicts a 60% chance of no live birth. There is still value in proceeding with additional cryopreservation cycles to optimize the chances of success, even if oocyte quality is above average.
- – Generate a VIOLET™ Summary report to understand cumulative blastocyst and live birth predictions over multiple cycles.
Summary: In this scenario, your patient’s oocyte quality is above average relative to general predictions. The VIOLET™ report may even predict a higher live birth rate with fewer frozen oocytes than you would typically recommend (i.e., evidence-based guidelines of freezing 20 oocytes for patients under 35). While these insights provide positive news to your patient, remind them that there are still many variables that need to be successful to reach a live birth.
You may decide to continue with a conservative treatment plan to freeze more oocytes over multiple cycles to maximize your patient’s chances of success. Even with a good prognosis scenario, there are still many variables that may impact success. Clinicians routinely encounter a similar situation with embryos, where failed euploid transfers occur 30-40% of the time.
If you would like to provide feedback on your counselling experience using this guidance, please share it with us at info@futurefertility.com.
Future Fertility Oocyte Software, including VIOLET™ reports and their personalized blastocyst and live birth predictions, have received the CE Mark as well as regulatory approval by the United Kingdom and Health Canada. This article is intended for clinicians who practice in regions where these approvals apply.
Future Fertility does its best to provide the most accurate results based on state-of-the-art technologies and software development. Outcome predictions may additionally be affected by suboptimal image quality.
REFERENCES
- Nayot D, Meriano J, Casper R, Krivoi A. 2020. An oocyte assessment tool using machine learning; Predicting blastocyst development based on a single image of an oocyte. 36th Annual Meeting of ESHRE – Copenhagen. https://futurefertility.com/wp-content/uploads/2022/11/ESHRE-2020-FF-Oocyte-assessment-tool-using-machine-learning-Predicting-blastocyst-development-based-on-oocyte-image.pdf.
- Goldman RH, Racowsky C, Farland LV, Munné S, Ribustello L, Fox JH. Predicting the likelihood of live birth for elective oocyte cryopreservation: a counseling tool for physicians and patients. Hum Reprod. 2017 Apr 1;32(4):853-859. doi: 10.1093/humrep/dex008. PMID: 28166330.
- Practice Committees of the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. Mature oocyte cryopreservation: a guideline. Fertil Steril. 2013 Jan;99(1):37-43. doi: 10.1016/j.fertnstert.2012.09.028. Epub 2012 Oct 22. PMID: 23083924.
- SART National Report 2016: ftp:/ftp.cdc.gov/pub/Publications/art/ART-2016-Clinic-Report-Full.pdf
- De Geyter C, Calhaz-Jorge C , Kupka MS, Wyns C, Mocanu E, Motrenko T, Scaravelli G, Smeenk J, Vidakovic S, Goossens V. The European IVF-monitoring Consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE), ART in Europe, 2015: results generated from European registries by ESHRE, Human Reproduction Open, Volume 2020, Issue 1, 2020, hoz038, https://doi.org/10.1093/hropen/hoz038.
- Doyle JO, Richter KS, Lim J, Stillman RJ, Graham JR, Tucker MJ. Successful elective and medically indicated oocyte vitrification and warming for autologous in vitro fertilization, with predicted birth probabilities for fertility preservation according to number of cryopreserved oocytes and age at retrieval. Fertil Steril. 2016 Feb;105(2):459-66.e2. doi: 10.1016/j.fertnstert.2015.10.026. Epub 2015 Nov 18. PMID: 26604065.
You Might Also Like …
Join our mailing list for dispatches on the future of fertility