STUDY QUESTION:
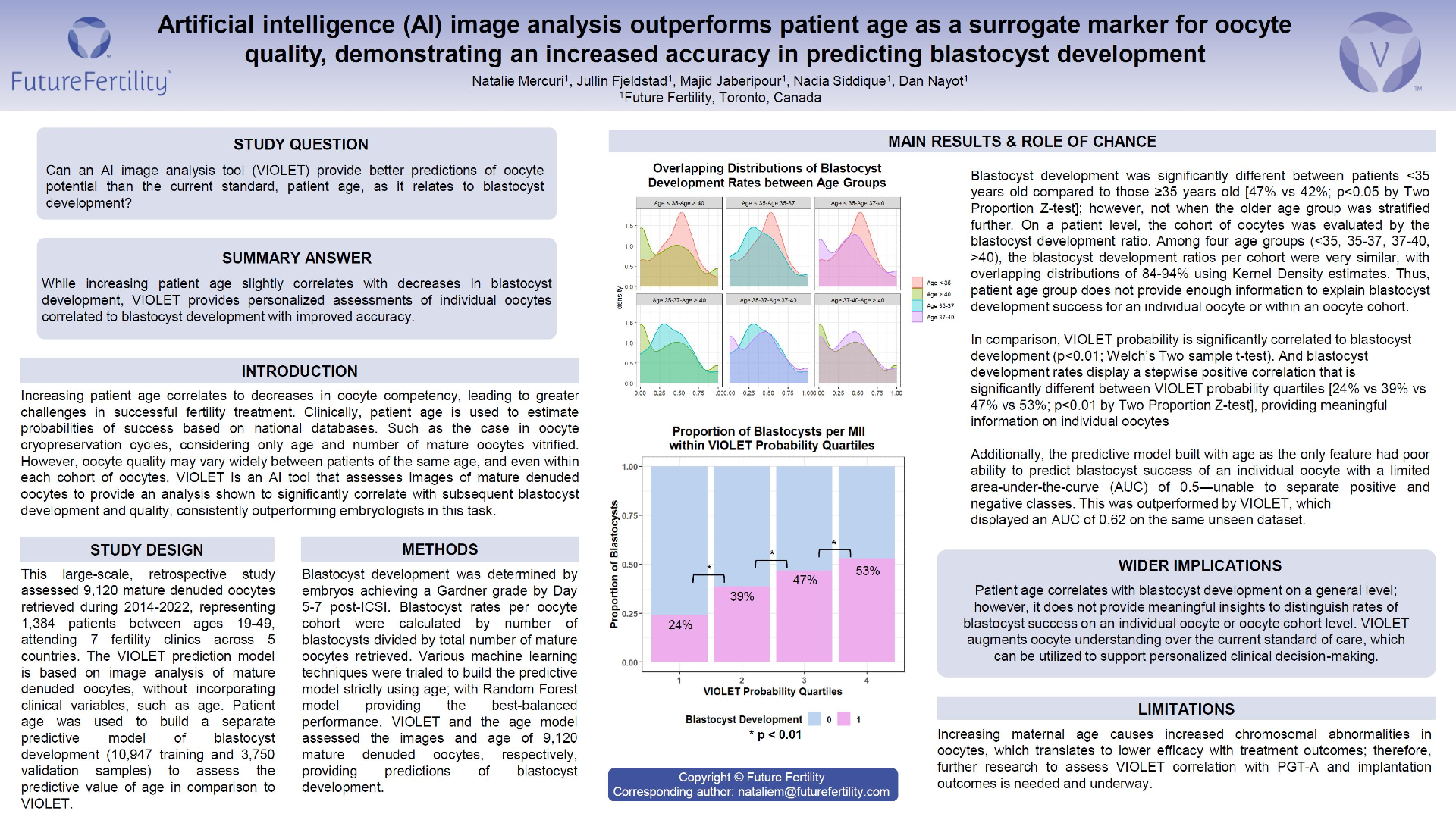
Can an AI image analysis tool (VIOLET) provide better predictions of oocyte potential than the current standard, patient age, as it relates to blastocyst development?
SUMMARY ANSWER:
While increasing patient age slightly correlates with decreases in blastocyst development, VIOLET provides personalized assessments of individual oocytes correlated to blastocyst development with improved accuracy.
WHAT IS KNOWN ALREADY:
Increasing patient age correlates to decreases in oocyte competency, leading to greater challenges in successful fertility treatment. Clinically, patient age is used to estimate probabilities of success based on national databases. Such as the case in oocyte cryopreservation cycles, considering only age and number of mature oocytes vitrified. However, oocyte quality may vary widely between patients of the same age, and even within each cohort of oocytes. VIOLET is an AI tool that assesses images of mature denuded oocytes to provide an analysis shown to significantly correlate with subsequent blastocyst development and quality, consistently outperforming embryologists in this task.
STUDY DESIGN:
This large-scale retrospective study assessed 9,120 mature denuded oocytes retrieved during 2014-2022, representing 1,384 patients between ages 19-49, attending 7 fertility clinics across 5 countries. The VIOLET prediction model is based on image analysis of mature denuded oocytes, without incorporating clinical variables, such as age. Patient age was used to build a separate predictive model of blastocyst development (10,947 training and 3,750 validation samples) to assess the predictive value of age in comparison to VIOLET.
METHODS:
Blastocyst development was determined by embryos achieving a Gardner grade by Day5/6 post-ICSI. Blastocyst rates per oocyte cohort were calculated by number of blastocysts divided by total number of mature oocytes retrieved. Various machine learning techniques were trialed to build the predictive model strictly using age; with Random Forest model providing the best-balanced performance. VIOLET and the age model assessed the images and age of 9,120 mature denuded oocytes, respectively, providing predictions of blastocyst development.
MAIN RESULTS AND THE ROLE OF CHANCE:
Blastocyst development was significantly different between patients <35 years old compared to those ≥35 years old [47% vs 42%; p<0.05 by Two Proportion Z-test]; however, not when the older age group was stratified further. On a patient level, the cohort of oocytes was evaluated by the blastocyst development ratio. Among four age groups (<35, 35-37, 37-40, >40), the blastocyst development ratios per cohort were very similar, with overlapping distributions of 84-94% using Kernel Density estimates. Thus, patient age group does not provide enough information to explain blastocyst development success for an individual oocyte or within an oocyte cohort.
In comparison, VIOLET probability is significantly correlated to blastocyst development (p<0.05; Welch’s Two sample t-test). And blastocyst development rates display a stepwise positive correlation that is significantly different between VIOLET probability quartiles [24% vs 39% vs 47% vs 53%; p<0.05 by Two Proportion Z-test], providing meaningful information on individual oocytes.
Additionally, the predictive model built with age as the only feature had poor ability to predict blastocyst success of an individual oocyte with a limited area-under-the-curve (AUC) of 0.5—unable to separate positive and negative classes. This was outperformed by VIOLET, which displayed an AUC of 0.62 on the same unseen dataset.
LIMITATIONS & REASONS FOR CAUTION:
Increasing maternal age causes increased chromosomal abnormalities in oocytes, which translates to lower efficacy with treatment outcomes; therefore, further research to assess VIOLET correlation with PGT-A and implantation outcomes is needed and underway.
WIDER IMPLICATIONS OF THE FINDINGS:
Patient age correlates with blastocyst development on a general level; however, it does not provide meaningful insights to distinguish rates of blastocyst success on an individual oocyte or oocyte cohort level. VIOLET augments oocyte understanding over the current standard of care, which can be utilized to support personalized clinical decision-making.
You Might Also Like …
Join our mailing list for dispatches on the future of fertility