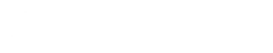
In IVF, oocyte selection may occasionally be required — whether due to regulations, clinical strategy, or patient preference. When only a subset of oocytes can be inseminated or thawed, the key clinical decision becomes how to select those with the highest developmental potential.
MAGENTA™ enables objective oocyte ranking, and retrospective analysis suggests that prioritizing higher-scoring oocytes can significantly improve blastocyst formation compared with random selection.
RETROSPECTIVE ANALYSIS USING MAGENTA™:
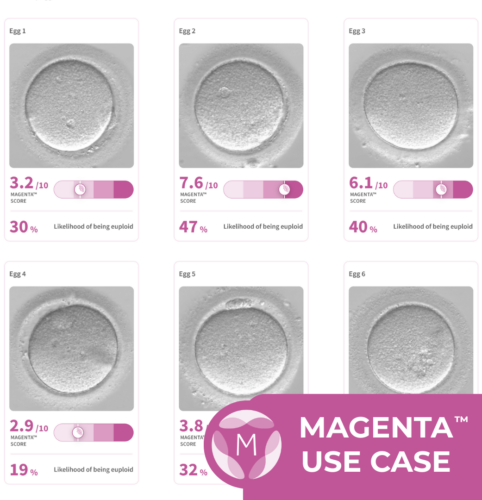
📊 To evaluate the potential impact of MAGENTA™-based oocyte ranking, our data science team conducted a retrospective analysis using new, unseen data.
- To isolate for scenarios in which oocyte selection may be considered, this analysis only includes cycles where >15 oocytes were retrieved
- 2,523 oocytes
- 139 cycles from 137 patients
- Oocytes were ranked using MAGENTA™ scores
- Outcomes were compared between
- Random selection of 3 oocytes
- Selection of the top 3 oocytes based on MAGENTA™ score
- Selecting the top 3 MAGENTA™-ranked oocytes resulted in a 27.6% relative increase in blastocyst development rate compared with random selection
WHEN OOCYTE RANKING MAY BE REQUIRED:
- Germany — Embryo Protection Act (Embryonenschutzgesetz): This act suggests only three oocytes may be fertilized per IVF cycle, and while practice may vary by clinic, this highlights the need for an objective assessment of oocytes. (Source)
- India — ART (Regulation) Act, 2021: Donor cycles are capped at seven oocytes per retrieval, creating an impact to equitable distribution across recipients. (Source)
- Patients who wish to avoid surplus embryos for personal reasons
- Operational or lab-capacity constraints, where very large cohorts create ICSI or culture bottlenecks
💡 In these cases, objective ranking helps ensure that the oocytes most likely to succeed are prioritized first.
CLINICAL VALUE OF MAGENTA™ OOCYTE RANKING:
- Introduces objectivity when selection is unavoidable: Provides a standardized, image-based approach to ranking oocyte quality rather than relying on subjective morphology or chance.
- Improves efficiency without increasing embryo numbers: Helps maximize blastocyst yield from a limited number of inseminated or thawed oocytes — particularly relevant in regulated environments.
- Supports transparent counselling and documentation: Enables clinicians to clearly explain why certain oocytes were prioritized, which can be especially important in donor allocation or ethically sensitive cases.
- Aligns with patient-centered care: Allows patients to proceed incrementally, using the oocytes most likely to succeed first while preserving future options.
THE BOTTOM LINE:
When oocyte selection is required — by regulation, clinical strategy, or patient preference — MAGENTA™ provides an objective, data-driven way to rank oocytes by developmental potential. Retrospective analysis suggests that prioritizing higher-scoring oocytes can meaningfully improve blastocyst outcomes, without increasing embryo creation or compromising patient values.
If you’ve found this example helpful in understanding how MAGENTA™ can be incorporated at your clinic or have feedback on other aspects related to your use of Future Fertility’s egg quality assessments, please share it with us at info@futurefertility.com.
You Might Also Like …
Join our mailing list for dispatches on the future of fertility