- Studies consistently rank oocyte quality as more influential than sperm characteristics or other variables in determining embryo morphology and pregnancy outcomes (Gangrade & Agarwal, 2013).
- Numerous studies consistently show that most embryonic aneuploidies arise from errors during maternal meiosis, with the risk increasing significantly as maternal age advances (Fragouli & Wells, 2014), (Chiang et al., 2012).
PATIENT CASE: UNEXPLAINED INFERTILITY
PATIENT BACKGROUND:
- A 28-year-old female G0P0 with primary infertility for 2.5 years presented for evaluation.
- Her ovarian reserve was below average, but not within the diminished range. A mild male factor was also identified.
- She previously failed low-level interventions, including four cycles of ovarian stimulation with intrauterine insemination (IUI).
- Given her overall favourable prognosis, she proceeded with in vitro fertilization (IVF).
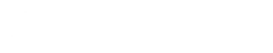
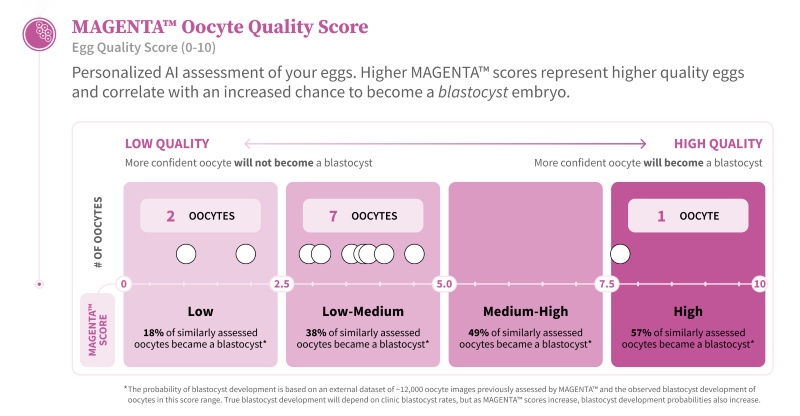
- The IVF cycle yielded 12 oocytes, 10 of which were mature (MAGENTA™ scores indicate that 90% of the oocytes are low scoring).
- The sperm sample had normal volume and concentration but motility was slightly reduced at 20%.
- Intracytoplasmic sperm injection (ICSI) resulted in fertilization of 8 oocytes. However, only one blastocyst developed that was frozen for an upcoming FET cycle.
Although the patient may still achieve success with her one frozen blastocyst, she and her partner recognize that the IVF cycle outcome was less favorable than expected based on their clinical profile. As expected, during their follow-up consultation, they had numerous questions aimed at better understanding the limited success of their cycle.
THE MAGENTA™ REPORT:
PATIENT COUNSELLING TIPS:
- Was the outcome related to the treatment protocol?
- Were the stimulation medications dosed too high or too low?
- Was the trigger administered on the appropriate day?
- Were any helpful adjuvant treatment medications not used to optimize outcomes?
- Could it have been due to IVF lab conditions?
- Was there an issue with sperm selection or ICSI technique by the embryologist?
- Could suboptimal culture media or conditions have impacted embryo development?
Internal Factors (Biology or Gametes)
- Was the result related to underlying sperm quality?
- Was the result related to underlying oocyte quality?
The MAGENTA™ report serves as a valuable counseling tool for physicians to help answer patient questions with objective insights on oocyte quality. Using MAGENTA™ to guide the discussion helps to:
- Provide patients with a clear understanding that oocyte quality likely played a significant role in the cycle’s limited success.
- Offer an objective, data-driven explanation for unexpected outcomes—particularly in younger patients—by highlighting a potential root cause of otherwise unexplained infertility.
- Reassure patients that the care they received aligned with current standards and best practices.
- Guide discussions around future options—such as pursuing another IVF cycle, with or without modifications to treatment based on the overall clinical picture.
If you would like to provide feedback on your counselling experience using this guidance, or cases of unexplained infertility using the MAGENTA™ report, please share it with us at info@futurefertility.com.
You Might Also Like …
Join our mailing list for dispatches on the future of fertility