THE PURPOSE OF MAGENTA™
MAGENTA™ reports provide you with individualized patient insights about oocyte quality to:
- • Better understand root cause of failed IVF-ICSI cycles:
- • Inform your decision-making on next steps and guide future cycle planning
- • Support counselling conversations following unsuccessful cycles
- • Manage patients’ expectations for success:
- • Compare versus standard of care estimations to help align patients to future treatment recommendations
HOW MAGENTA™ REPORTS WORK TO STANDARDIZE OOCYTE ASSESSMENT
Future Fertility technology uses AI to assess 2D images of fresh denuded mature (MII) oocytes – detecting features invisible to the human eye – to provide a MAGENTA™ score. The MAGENTA™ score is based on the oocyte’s reproductive potential; more specifically, it represents the oocyte’s likelihood to develop into a blastocyst.
Currently, there is no validated oocyte visual scoring system (ALPHA 2011) to be able to provide consistent and objective feedback on oocyte quality. Our model was built using more than 120,000 oocyte images and their lab outcomes from partnering clinics across eight countries. Our AI consistently outperforms the accuracy of embryologists in predicting blastocyst formation by at least 20%, on average.1
Our integration and validation with EmbryoScope (time-lapse incubator) and other light microscope cameras/lasers make MAGENTA™ easy to adopt into the lab workflow and integrate into clinical practice.
THE NEED FOR OOCYTE QUALITY PREDICTIONS IN ICSI
Gaining individualized oocyte quality insights fills a critical gap in the IVF-ICSI treatment process. While there are ways to assess sperm quality and embryo quality, information about the oocyte is limited within the current standard of care (number, nuclear maturity, age-related predictions). Given the overall high cycle failure rates, managing patient expectations throughout the process becomes paramount in encouraging them to consider serial attempts, thereby increasing their cumulative chances of success.
Furthermore, information about the oocyte can aid in identifying potential contributing factors to treatment failure, thus supporting personalized future cycle planning and improving overall patient care.
Labs routinely use similar technologies and grading approaches to measure sperm and embryo quality. Failed ICSI with morphologically normal motile sperm and failed embryo transfers of high-quality euploid embryos are unfortunately part of routine practice.
MAGENTA™ should be considered an addition to this toolkit to provide improved insights on the current IVF-ICSI cycle and be used as a counselling tool to optimize future cycle planning. While MAGENTA™ reports consistently outperform embryologists’ predictive ability, this AI technology is still evolving and is not 100% accurate.
Below we will walk you through how to use MAGENTA™ in a variety of counselling scenarios to better demonstrate the role this can play in patient care.
WHAT’S IN THE REPORT?
MAGENTA™ reports provide an objective measure of oocyte quality, including individual oocyte images and their predictions of blastocyst formation using scores on a scale of 0-10. The assigned score correlates with the reproductive potential of an oocyte to develop into a blastocyst – the higher the MAGENTA™ score, the more likely it is that the oocyte will develop into a blastocyst. We’ve conducted prospective studies in multiple regions with trusted clinical partners, all of which have validated the technology and demonstrated the model’s positive correlation.
- • The front page of the MAGENTA™ report provides a visual summary of MAGENTA™ scores for the full cohort of oocytes evaluated.
- • At the bottom of the first page, you can understand the observed Blastocyst Rate for each MAGENTA™ score range.
- • The remaining pages provide individual oocyte images alongside their respective MAGENTA™ scores.
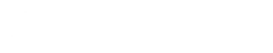
COUNSELLING SCENARIOS
When using MAGENTA™ reports to counsel your patients, our recommendation is to focus on comparing the personalized insights to generalized expectations (based on age and reproductive history) to either:
- • Confirm expectations and treatment decisions, or;
- • Modify expectations and identify opportunities to adjust future treatment cycles.
In all scenarios, MAGENTA™ reports function as an empirical and tangible tool to better manage your patients’ expectations based on their personal oocyte quality and help you determine future treatment options. Empowering patients with personalized insights provides greater transparency. This can improve their trust and satisfaction with the clinic, thus reducing the risk of patients seeking future treatment at competitive clinics.
It’s important to highlight that MAGENTA™ scores should not be interpreted as a reflection of lab performance, even in the case of unsuccessful cycles with high-quality oocytes.
1. MAGENTA™ SCORES INDICATE LOW-QUALITY OOCYTES, AS EXPECTED:
Counselling actions and next steps:
- • Confirm standard of care expectations with your patient:
- • Share with your patient that their personalized oocyte assessment is consistent with expectations based on their age and reproductive history.
- • Provide transparency to your patient by highlighting their personalized insights regarding low oocyte quality to help manage their expectations of success.
- • Enabling the patients to visualize these scores and images of their eggs can help them to accept this news and align with recommendations for future treatment options.
- • Consider another IVF-ICSI cycle, with interventions or adjustments that may help optimize oocyte quality (e.g., dietary supplements, lifestyle changes, treatment protocol adjustments, etc.)
- • Consider egg donation as a possible next step.
- • You may decide to provide a copy of the MAGENTA™ report to the patient that they may take home as documentation of their oocyte quality.
Summary: If a cycle fails or if blastocyst development results are lower-than-expected, clinicians can use MAGENTA™ scores to reinforce expectations about low oocyte quality due to patient age or reproductive history. We expect this to be the most common use case for MAGENTA™ in your clinic (e.g., advanced female age, previous failed IVF cycles, etc.). The report provides you and your patient with a tangible document to help guide the conversation, helping the patient to better understand a possible cause of failure and exploring feasible next steps.
2. MAGENTA™ SCORES INDICATE HIGH-QUALITY OOCYTES, AS EXPECTED:
Counselling actions and next steps:
- • Confirm standard of care expectations with your patient:
- • Share with your patient that their personalized oocyte assessment is consistent with expectations based on their age and reproductive history.
- • Leverage the report to support the case for additional cycles, along with the potential optimization of other factors (e.g., sperm quality, uterine factor)
- • You may decide to provide a copy of the MAGENTA™ report to the patient that they may take home as documentation of their oocyte quality.
Summary: If a cycle fails or if blastocyst results are lower-than-expected, clinicians can use MAGENTA™ scores to confirm high oocyte quality expectations with the patient. These scores support the case for additional cycles, given the patient’s likelihood of success, along with the optimization of other factors for future treatment cycles.
3. MAGENTA™ SCORES INDICATE UNEXPECTED LOW-QUALITY OOCYTES:
Counselling actions and next steps:
- • Inform your patient that their oocyte quality is lower than expected:
- • Share with your patient that their personalized oocyte assessment was lower than expected based on their age and reproductive history. If the cycle was unsuccessful, you can show your patient how the outcomes are aligned with the AI’s assessment of low oocyte quality.
- • Providing transparency to your patient by highlighting their personalized insights regarding low oocyte quality enables you to better manage their expectations of success for future cycles.
- • Enabling the patients to visualize these scores and images of their eggs can help them to accept this news and align with recommendations for future treatment options.
- • Identify oocyte quality issues early to optimize future cycles sooner vs. assuming other factors are the main drivers.
- • If the cycle is not successful, recommend additional cycles and consider interventions or adjustments that focus on oocyte quality.
- • At your discretion, consider egg donation as a future treatment option.
Summary: Clinicians can use MAGENTA™ reports to highlight low oocyte quality during counselling conversations for unsuccessful cycles, and optimize future treatment. By providing personalized patient insights, these reports promote transparency and help align patients with recommendations for future treatment. Ultimately, this can improve patients’ satisfaction with clinic services, leading to increased patient retention for the clinic.
4. MAGENTA™ SCORES INDICATE UNEXPECTED HIGH-QUALITY OOCYTES:
Counselling actions and next steps:
- • Inform your patient that their oocyte quality is higher than expected:
- • Share with your patient that their personalized oocyte assessment is higher than expectations based on their age and reproductive history.
- • Although age is a strong predictor of oocyte quality in the general public, there is a wide variation among patients of the same age. While your patient has higher-than-expected oocyte quality, this still does not mean success is guaranteed (see next point).
- • Continue to manage your patient’s expectations, as multiple variables contribute to ultimate success:
- • While MAGENTA™ reports are better than embryologists at predicting blastocyst outcomes for oocytes, this AI technology is still evolving and is not 100% accurate.
- • If the cycle is unsuccessful, other factors may need more consideration (e.g., sperm quality, uterine factor)
Summary: In learning that oocyte quality is higher than expected, clinicians can focus on optimizing other factors to help improve future cycle outcomes. Clinicians may share this good news with the patient while continuing to caution that other factors may still impact cycle outcomes that are not reflected in the MAGENTA™ score (for instance, other age-related factors that could impact success).
If you would like to provide feedback on your counselling experience using this guidance, please share it with us at info@futurefertility.com.
Future Fertility Oocyte Software, including VIOLET™ reports and their personalized blastocyst and live birth predictions, have received the CE Mark as well as regulatory approval by the United Kingdom and Health Canada. This article is intended for clinicians who practice in regions where these approvals apply.
Future Fertility does its best to provide the most accurate results based on state-of-the-art technologies and software development. Outcome predictions may additionally be affected by suboptimal image quality.
REFERENCES
- Nayot D, Meriano J, Casper R, Krivoi A. 2020. An oocyte assessment tool using machine learning; Predicting blastocyst development based on a single image of an oocyte. 36th Annual Meeting of ESHRE – Copenhagen. https://futurefertility.com/wp-content/uploads/2022/11/ESHRE-2020-FF-Oocyte-assessment-tool-using-machine-learning-Predicting-blastocyst-development-based-on-oocyte-image.pdf.
You Might Also Like …
Join our mailing list for dispatches on the future of fertility