You’ve probably heard the term ovarian reserve and you may also have an idea of what your personal reserve is. Even with this knowledge, have you found yourself wondering – what does my ovarian reserve tell me about my fertility? How important is this factor while trying to conceive? Is there anything I can do to improve or preserve my reserve over time?
In this blog, we are diving into common misconceptions surrounding the topic and shedding light on the various factors that influence it.
Let’s start with a definition. Ovarian reserve refers to the quantity of oocytes, or eggs, in the ovaries, but not necessarily their quality. Understanding your own ovarian reserve can provide valuable insights as you navigate family planning.
MYTH #1: Age is the Sole Determinant of Ovarian Reserve
We know that age is an important factor when it comes to your fertility. As we age, the number and quality of eggs in our ovaries naturally decline.
However, it’s necessary to recognize that age is not the only factor impacting your oocyte supply. There are many influences including genetics, autoimmune conditions, medical treatments (like chemotherapy, radiation on the pelvis, or surgery on the ovaries), lifestyle choices (smoking, excessive alcohol intake, obesity), and even environmental conditions present during follicular development (while you were still in the womb!) that can affect ovarian reserve.¹
One of the best approaches to support your ovarian reserve, or slow down its decline, is to minimize exposure to negative impacts. You may not be able to control biological aging and you can’t choose your genetic profile, but you can create lifestyle habits that will benefit your ovarian reserve, like choosing not to smoke.
While it’s true that there’s a large biological variability in egg quality and quantity at each age, both inevitably decrease over time. Even the most fertile among us may eventually face fertility challenges while trying to conceive, and will transition into menopause at some point.

Graphic adapted from “Potential factors result in diminished ovarian reserve: a comprehensive review”, Zhu et al. 2023, Journal of Ovarian Research.
MYTH #2: Ovarian Reserve Only Concerns Those Actively Trying to Conceive
You are born with all the eggs that you will have in your lifetime. Unlike how males create sperm, females do not generate new eggs, and with time, egg count naturally decreases.
Because there is no way to reverse natural egg loss, having an idea of your own ovarian reserve can provide valuable insights to your overall reproductive health and help you make family planning decisions – even if you are not yet trying to conceive.
Clinically, ovarian reserve testing is used to predict how well you may respond to ovarian stimulation during an egg retrieval.² This is an important marker for success in IVF and egg freezing treatments. In general, the more eggs you retrieve in a cycle, the more opportunities you will have to create viable embryos. Of course, a single high-quality egg is better than many low-quality eggs, but statistically speaking, having a higher reserve will improve your overall chance of success.
If you’re curious about your own ovarian reserve, work with your OBGYN or a fertility specialist to conduct a fertility evaluation involving bloodwork and an ultrasound.
The blood tests measure your hormone levels – specifically, anti-Mullerian hormone (AMH) and follicle-stimulating hormone (FSH). This is generally done in the early phase of your cycle (day 2-4).
FSH and AMH are found in both men and women but play different biological roles in the body. In women specifically, FSH helps to regulate the menstrual cycle by stimulating follicles on the ovary to grow and prepare for ovulation. AMH is produced and secreted by the ovarian follicles as they grow and work to support the ovulation process.
The ultrasound component of this testing looks at the follicles present on your ovaries to provide your antral follicle count (AFC). Taken together, the AMH, FSH and AFC make up your ovarian reserve evaluation.
For instance, a lower reserve is indicated by a high FSH level and low AMH and AFC.³ If someone receives this information before they are ready to conceive, it may prompt them to consider egg freezing to preserve remaining eggs. On the other hand, receiving this information while going through IVF helps patients and clinicians tailor treatment approaches.
MYTH #3: Quality vs. Quantity – Low Ovarian Reserve is Always Indicative of Infertility
Perhaps you’ve already undergone a fertility work-up, or you may have even heard your doctor say something along the lines of “You have the eggs of a 26-year-old!” In most cases, they’re referring to the number of eggs in your reserve, not the quality of those eggs. Meaning, you can have an indication of how many eggs you may have, but not necessarily know the health of those eggs.
For example, people with polycystic ovary syndrome (PCOS) are expected to have a higher antral follicle count and may retrieve more eggs than the average patient. (PCOS is a term used when the AFC is 12 or more on each ovary.) However, some studies suggest that patients with PCOS have lower-quality eggs, especially notable when patients are older.4
Conversely, you may already know that you have a diminished ovarian reserve (DOR) and think that means you are infertile. Fortunately, this is a persistent myth, and is not necessarily the case. Studies consistently show that having DOR doesn’t impact your natural fertility, since in a natural cycle you are only releasing one egg at a time anyway, regardless of your reserve. It is true, though, that DOR can decrease your chances of success with fertility treatments such as IVF where more eggs generally lead to a higher success rate.
Traditionally, age has been the main factor in estimating egg quality, and ovarian reserve testing has been used to reflect egg quantity. Putting these together, a young patient with DOR is expected to have few high-quality eggs, whereas an older patient with a high reserve is expected to have many low-quality eggs. However, both cases may still lead to success.
You can gain a general estimate of your chances of success using an online egg calculator – this is helpful if you’re looking for directional information prior to an egg retrieval. However, these estimates are based on population health statistics that only consider age and the number of mature eggs retrieved, without factoring in your personal health situation.
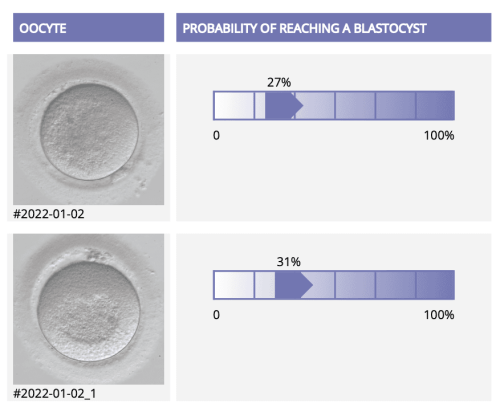
To gain more precise insight into the quality of your own eggs, ask your clinic in advance of your egg retrieval about receiving a personalized egg quality report. VIOLET™ reports (for egg freezing patients) and MAGENTA™ reports (for IVF patients) leverage AI technology to analyze images of each egg taken by the fertility clinic’s lab after a retrieval to assess their likelihood of developing into a blastocyst (a day 5-6 embryo). Beyond your ovarian reserve results, understanding the quality of your eggs equips you and your fertility care team to make more informed decisions about your treatment.
We hope that by debunking these myths around ovarian reserve you feel empowered to make informed choices for your reproductive health. Age is a factor, but it’s not the only one. Knowing the various influences on your ovarian reserve allows you to make lifestyle decisions and plan proactively. Whether you are curious about freezing your eggs or are already along the path to IVF, understanding your ovarian reserve will help you better navigate decisions about your own future fertility.
1 https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-023-01296-x
2 https://my.clevelandclinic.org/health/diagnostics/25142-ovarian-reserve-testing
3 https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/j.1600-0412.2012.01471.x
4 https://www.centerforhumanreprod.com/blog/pcos-effects-on-egg-quality-are-age-dependent
You Might Also Like …
Join our mailing list for dispatches on the future of fertility