What is PCOS?
Polycystic Ovary Syndrome (PCOS) is a hormonal disorder that many women experience during their reproductive years. It’s caused by an imbalance in hormones—often higher levels of androgens (male hormones)—which can interfere with regular periods, ovulation, and fertility. While common, PCOS is manageable, and learning how it affects your body is an important first step.
What Causes PCOS?
The exact cause isn’t fully understood, but research suggests a mix of genetic and environmental factors (source). Key contributors include:
- Insulin resistance – when the body doesn’t respond properly to insulin, leading to higher insulin levels and increased androgen production
- Hormone imbalances – elevated androgen levels can affect aspects of ovulation
- Inflammation – low-grade inflammation has been linked to PCOS symptoms
How Does PCOS Affect Health and Fertility?
PCOS can influence various aspects of a woman’s health, including:
- Menstrual cycle – irregular or absent periods
- Fertility – irregular ovulation, making it more difficult to get pregnant
- Metabolic health – higher risk of obesity, type 2 diabetes, and cardiovascular disease
- Mental health – increased rates of anxiety and depression
How Common is PCOS?
PCOS is one of the most common endocrine disorders among women of reproductive age, affecting an estimated 6-13% of women worldwide (source). Despite its prevalence, many women remain undiagnosed or unaware of the condition, highlighting the importance of awareness and education.
How do I know if I have PCOS?
Because PCOS symptoms can look different for everyone, many women may not realize they have the condition until they experience fertility challenges. Common symptoms include:
- Irregular periods – long, unpredictable, or absent cycles
- Acne
- Excessive hair on the face or body (hirsutism)
- Hair thinning or male-pattern balding
- Changes in weight
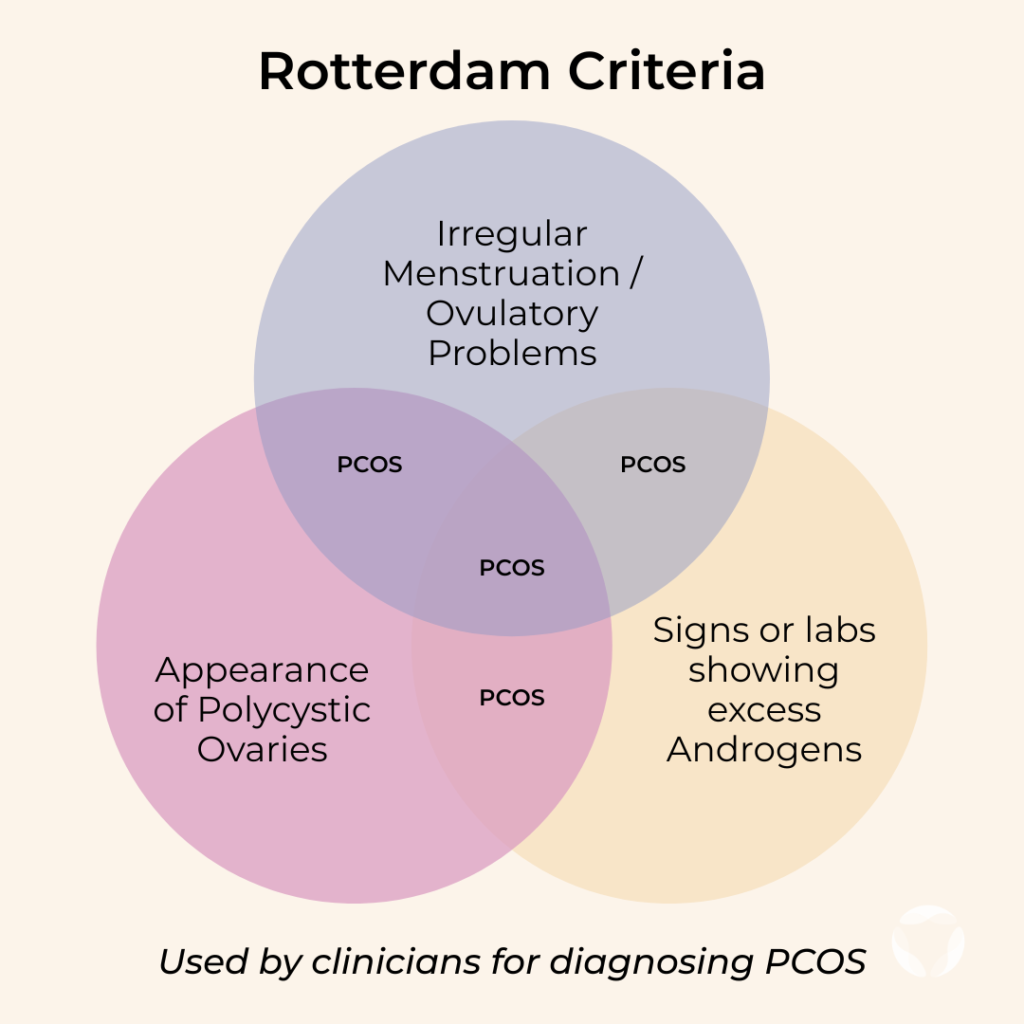
While it’s helpful to be aware of these symptoms, the best first step is to speak with a clinician. PCOS diagnosis usually involves blood tests to check hormone levels and an ultrasound to look at ovarian follicles — the small fluid-filled sacs that contain immature eggs.
Clinicians typically use the Rotterdam criteria when evaluating PCOS. To be diagnosed, a patient must present with at least two of the following: problems with ovulation, elevated androgens, or polycystic ovaries. (Source)
Can Women with PCOS Freeze Their Eggs?
Yes. Women with PCOS can undergo egg freezing, and for many, it can be a beneficial option. Egg freezing allows you to preserve eggs at a younger age, when they are more likely to be of higher quality, for use in the future when you’re ready to try for pregnancy. Women with PCOS often have a higher ovarian reserve and will respond to fertility medications by producing more follicles than non-PCOS fertility patients.
However, it’s important to approach egg freezing with realistic expectations:
- Women with PCOS commonly retrieve a higher number of eggs.
- More eggs don’t always mean greater success – egg quality, not just count, is what matters for fertility.
- PCOS patients may be at slightly higher risk of ovarian hyperstimulation syndrome (OHSS) during fertility treatments, so careful monitoring by your clinical team is essential.
This brings us to a crucial consideration, egg quality.
PCOS and Egg Quality

Quality plays a big role in whether an egg can develop into a high-quality embryo and result in a successful pregnancy.
Although women with PCOS might retrieve more eggs, studies suggest that their eggs may have lower quality, especially as women age (source). This can be due to hormonal imbalances affecting the maturation and release of eggs, (source).
The success of fertilization, embryo growth, and implantation depends strongly on egg quality.
IVF with PCOS: Making Sense of Outcomes
As we’ve seen, women with PCOS often respond strongly to fertility medications and can retrieve many eggs during IVF. But because egg quality varies, the number of embryos that develop may be lower than expected, leaving patients frustrated and confused when they were initially hopeful about the high egg retrieval count.
If you want to see a real-world example, check out this case study of a PCOS patient using MAGENTA™ to gain clearer understanding of her egg quality.
How You Can Learn About Your Egg Quality with AI
Traditionally, doctors have estimated fertility based on age and the number of mature eggs retrieved. But for women with PCOS, this can be misleading, since quantity is usually high, but quality may vary.
This is where advanced technologies like AI-powered egg quality assessment can play a supportive role. By analyzing images of your eggs, AI can detect subtle patterns and characteristics that predict the egg’s potential to grow into a high-quality blastocyst (day 5-7 embryo).
This kind of personalized insight goes beyond age-based averages, helping women gain a clearer picture of their unique egg quality and make more informed decisions about their fertility options.
To gain more precise insight into your own egg quality, ask your clinic in advance of your egg retrieval about receiving a personalized VIOLET™ report for egg-freezing or MAGENTA™ report for IVF/ICSI.
You Might Also Like …
Join our mailing list for dispatches on the future of fertility