In patients with polycystic ovary syndrome (PCOS), IVF generally results in a high number of retrieved oocytes. Clinicians and patients may initially feel optimistic about the large cohort size—however, these cycles can result in lower-than-expected blastulation rates or embryo quality, leading to patient confusion and frustration.
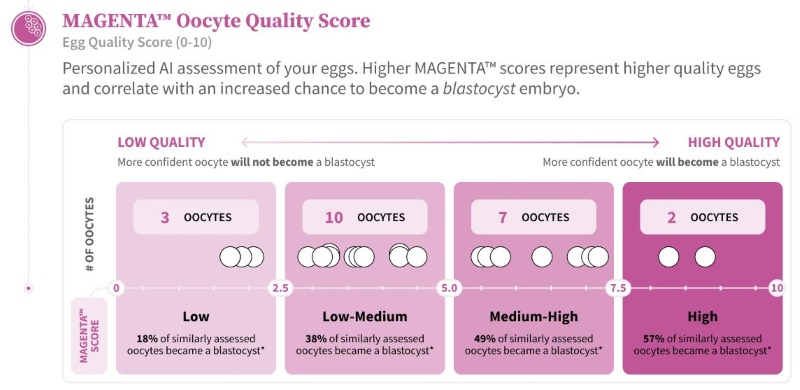
Traditional clinic metrics like AMH and antral follicle count predict quantity, but not quality. That’s where MAGENTA™ can add clinical value.
SAMPLE PATIENT CASE:
PATIENT BACKGROUND:
- A 34-year-old female G0P0; Primary infertility; TTC > 2 years with classic lean PCOS phenotype (irregular cycles, polycystic ovarian morphology, BMI 27).
- AMH 8.2 ng/mL; AFC >40.
- She previously failed low-level intervention, including numerous cycles of ovulation induction with IUI treatment.
- Patient underwent antagonist protocol with 150 IU FSH daily, triggered with GnRH agonist to avoid OHSS, and a freeze all approach.
- The IVF cycle yielded 27 oocytes, 22 of which were mature. MAGENTA™ scores indicate that 59% (13/22) of the mature oocytes were categorized in the low or low-medium quality.
- Semen analysis was within normal range.
- Of the 22 mature oocytes, 18 fertilized successfully via ICSI. A total of 7 embryos developed into early blastocysts, but 2 arrested before Day 6, resulting in 5 blastocysts that were frozen.
HOW MAGENTA™ INSIGHTS PROVIDE VALUE:
- Supports patient counselling conversations:
- Offers further insight into the patient’s specific reproductive potential of their high-yield cohort—revealing whether the egg quality is aligned with the patient’s high expectations.
- Helps explain why patients with PCOS, despite having a good ovarian response, may not achieve expected blastulation outcomes.
- Supports clinical decision-making for future cycles—whether through pre-treatment preparation before another IVF attempt or protocol adjustments in a subsequent cycle.
THE MAGENTA™ REPORT:
CLINICAL DECISION SUPPORTED BY MAGENTA™:
The clinician used this data to counsel the patient that, while there was a good ovarian response as expected, underlying challenges with oocyte quality (evidenced by the low scores for 13/22 oocytes in the MAGENTA™ report) likely limited the outcomes relative to pre-treatment expectations
PATIENT COUNSELLING TIPS:
- Explain that PCOS is often associated with compromised oocyte competence. [See references below.]
- Use MAGENTA™ to reframe the discussion, helping the patient understand that only a subset of mature oocytes have the reproductive potential to reach a viable embryo.
- Reassure patients that the insights can guide more targeted and personalized cycles going forward.
- Some considerations may include:
- Managing hyperandrogenism prior to a 2nd IVF attempt (e.g., medical and lifestyle optimization).
- IVF protocol adjustments (e.g., lower dosing of gonadotropins to decrease the ovarian stimulation response).
- Some considerations may include:
If you would like to provide feedback on your counselling experience using this guidance, or cases of PCOS using the MAGENTA™ report, please share it with us at info@futurefertility.com.
REFERENCES
- Altered Cytoplasmic Maturation and Mitochondrial Dysfunction
- A 2024 review by Yan et al. in Reproductive Biology and Endocrinology discusses mitochondrial dysfunction in granulosa cells (GCs) of PCOS patients. It highlights structural abnormalities, impaired mitochondrial function, and reduced mitochondrial membrane potential, all of which compromise GC functionality and oocyte quality.
- Reference: Oxidative stress and energy metabolism abnormalities in polycystic ovary syndrome: from mechanisms to therapeutic strategies | Reproductive Biology and Endocrinology | Full Text
- Disrupted Cumulus-Oocyte Communication
- Wood et al. (2007) in Human Reproduction Update reported altered gene expression in metaphase II (MII) oocytes from PCOS patients, particularly involving genes related to the maternal zygotic transition and the mitotic cell cycle. These changes suggest disrupted communication between cumulus cells and oocytes, affecting oocyte maturation and developmental competence.
- Reference: Pathology of Hyperandrogenemia in the Oocyte of Polycystic Ovary Syndrome – PMC
- Oxidative Stress in PCOS Oocytes
- A 2024 study by Yan et al. in Reproductive Biology and Endocrinology emphasizes that mitochondrial dysfunction and increased oxidative stress in GCs are pivotal contributors to aberrant follicular development and impaired fertility in PCOS patients. These factors collectively lead to compromised oocyte quality.
- Reference: Oxidative stress and energy metabolism abnormalities in polycystic ovary syndrome: from mechanisms to therapeutic strategies | Reproductive Biology and Endocrinology | Full Text
- Lower Developmental Competence Despite High Yield
- Dumesic et al. (2008) in Fertility and Sterility noted that although PCOS patients often retrieve more oocytes during IVF, these oocytes frequently exhibit reduced developmental competence, leading to lower fertilization and implantation rates.
- Reference: Polycystic Ovary Syndrome and Oocyte Developmental Competence – PMC
Join our mailing list for dispatches on the future of fertility